These programs are not insurance plans and do not provide full coverage. State of California established under the federal Patient Protection and Affordable Care Act.
 Covered California Medicare Notices Health For California
Covered California Medicare Notices Health For California
If you are uninsured and are not eligible for Medi-Cal or a plan through Covered California you may qualify for limited health services offered by your county.
Covered california not eligible. If you do not find an answer to your question please contact your local county office from our County Listings page or email us. Covered California is the new marketplace that makes it possible for individuals and families to get free or low- cost health insurance through Medi-Cal or to get help paying for private health insurance. Immigrants who are not lawfully present are not eligible to purchase a Covered California Health Plan.
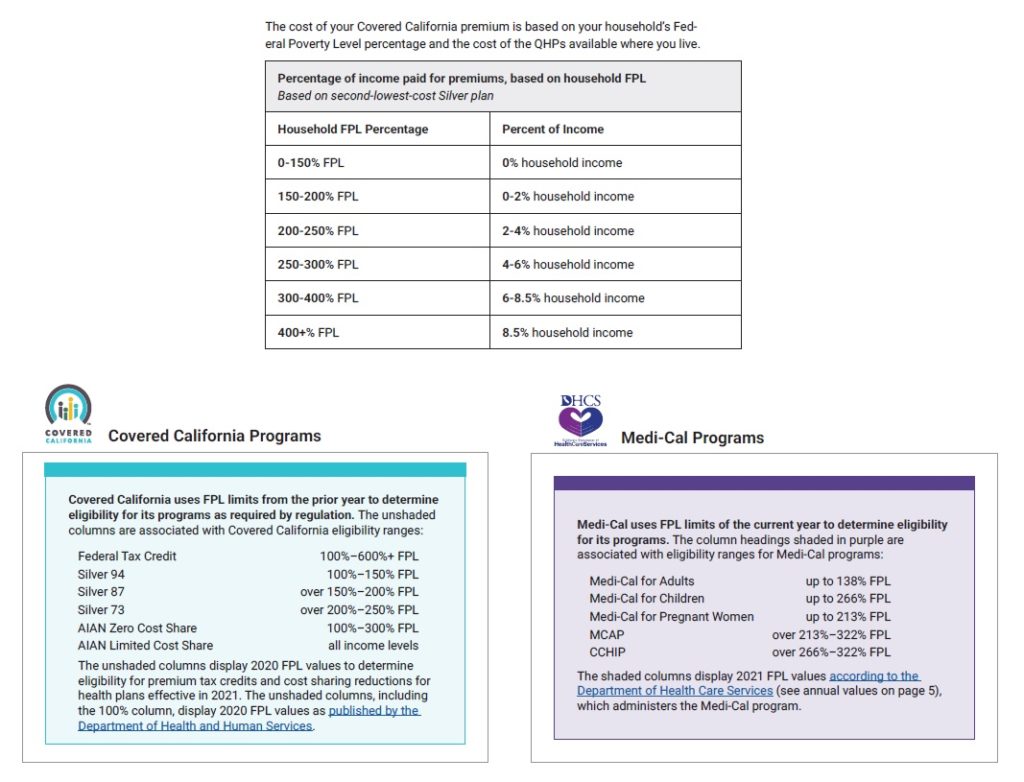
Covered California is a partnership of the California Health Benefit Exchange and the California Department of Health. Family members on your Covered California plan who arent eligible for Medicare can stay on the Covered California plan and continue to get financial assistance if eligible. In order to be eligible for assistance through Covered California you must meet an income requirement.
Back to Medi-Cal Eligibility. Medi-Cal Eligibility and Covered California - Frequently Asked Questions. Both lawfully present and not lawfully present individuals can apply through Covered California to see if they are eligible for a health plan through Covered California or Medi-Cal.
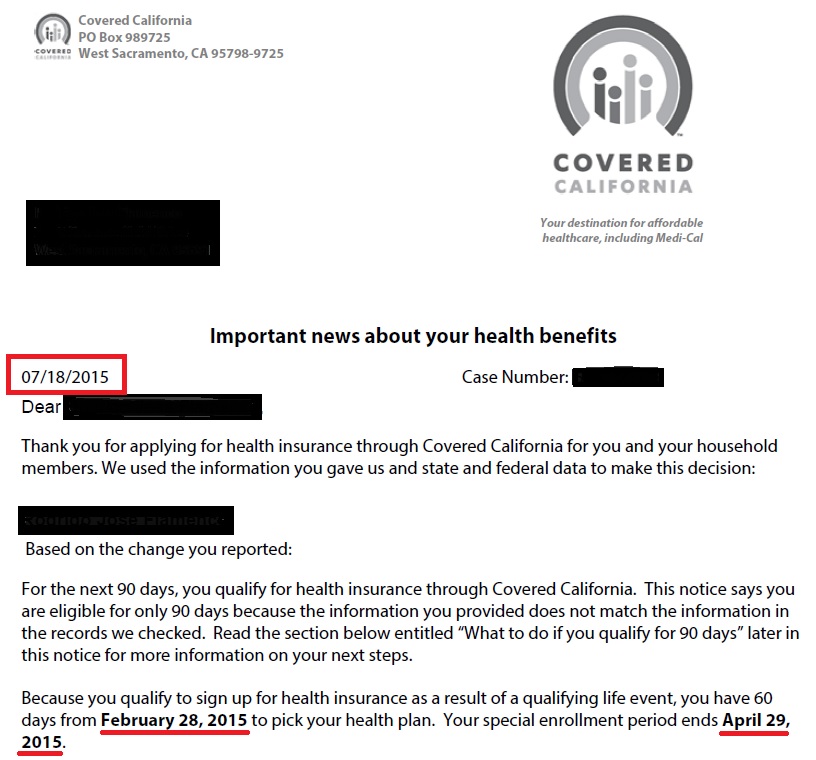
There is no waiting period or five-year bar. For questions about CCSB eligibility please contact covered California for Small Business at 844 332-8384 Monday through Friday between 800 am. You currently have a Covered California plan and become eligible or ineligible for cost sharing reductions or tax credits.
When applying remember that family members who are not lawfully present are not eligible for Covered California health plans but may be eligible for Medi-Cal. If you make 601 of the FPL you will be ineligible for any subsidies. Deferred Action for Childhood Arrivals DACA individuals are not considered legally present in the US.
However they may qualify for coverage through Medi-Cal up. Additionally Medicare supplement insurance Medigap plans will not be offered through Covered California. The benefits will be reversed however if the subsidies disappear in 2023 and are not made permanent.
Immigrants not considered to be lawfully present do not. If you are a sole proprietor with no W-2-receiving employees you may be eligible to purchase coverage through Covered Californias individual marketplace. Individuals who are eligible for Medicare will not be eligible to receive premium assistance through Covered California.
County health programs are commonly known as county indigent health or programs medically indigent adult programs. Our goal is to make it simple and affordable for Californians to get health insurance. Below you will find the most frequently asked questions for current and potential Medi-Cal coverage recipients.
Even if youve checked before check again because more than a million people could see more savings. However their eligibility must go through the determination process again which may change the amount of financial assistance they can receive. The exchange enables eligible individuals and small businesses to purchase private health insurance coverage at federally subsidized rates.
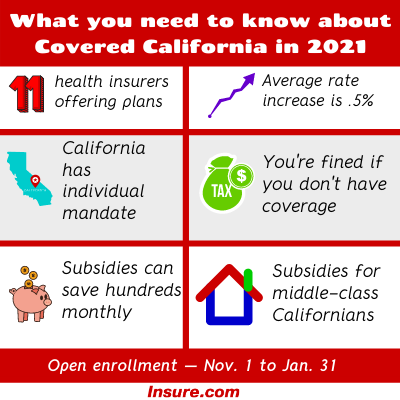
Covered California is the health insurance marketplace in the US. In order to qualify for federal tax credits or a subsidy in California you must make between 0-600 of the FPL. The California health insurance penalty is reinstated which means most Californians who choose not to buy qualified health insurance will face a tax penalty There is a new state subsidy program that is expected to help 235000 Californians who previously did not qualify for federal assistance.
They are however required to pay a tax penalty if they do not have any health insurance. And 500 pm or email smallbusinesscoveredcagov. Ninety percent of people who have enroll with Covered California get financial help and you could be one of them.
You could even qualify for low-cost or free health coverage through Medi-Cal. We project Covered California will enroll 135000 who would otherwise be uninsured leaving 630000 uninsured but eligible for subsidies in 2022. See If Youre Eligible for Financial Help.
As such they are not eligible for Covered California. When you applied misconduct or misinformation occurred on the part of your authorized representative or incorrect eligibility or plan information occurred during enrollment. It is administered by an independent agency of the government of California.
Covered California plan selection functionality is enabled by the County Eligibility Worker. If an Agent or CEC would like to confirm a consumer in Soft Pause contact Covered California Certified. The consumer or their Medi-Cal Authorized Representative can contact the county and request the completion of eligibility updates and Soft Pause review.
Immigrants who are not lawfully present do not qualify for a health plan through Covered California. Noncitizens that are not lawfully present you can still apply for health care through Covered California. However they can still apply through Covered Califor-nia to see if they may be eligible to receive low or no-cost coverage through Medi-Cal.