Anthem Blue Cross Blue Shield prescription drug benefits include medications available on the Key Advantage Drug List. Anthem Blue Cross and Blue Shield is the trade name of.
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
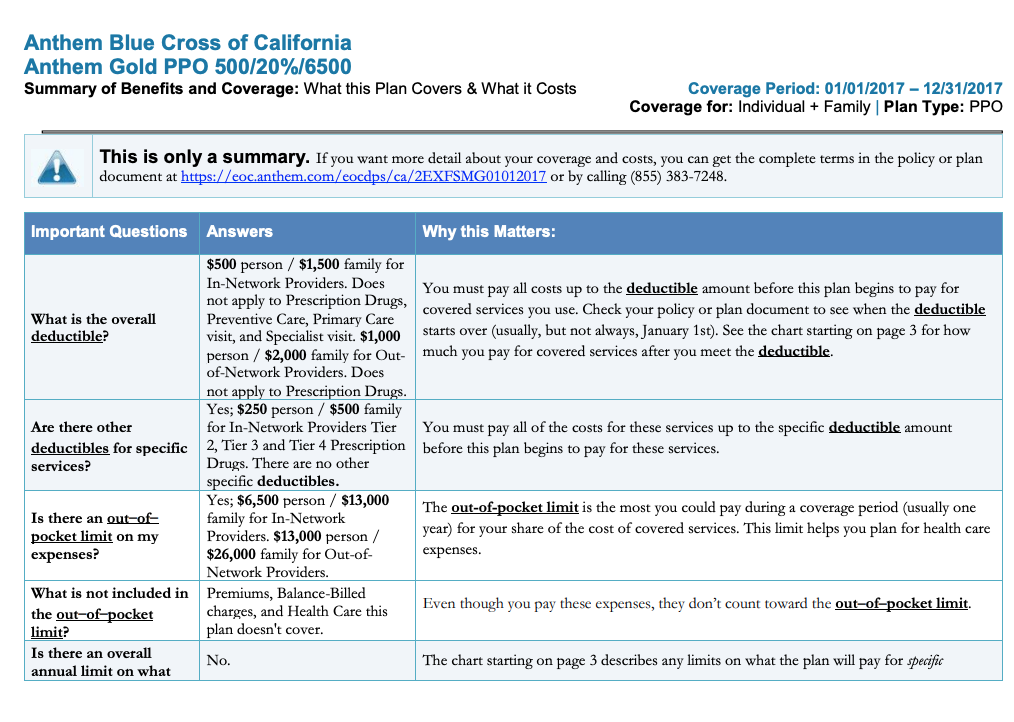
Check with your employer to make sure you have Anthem Blue Cross or Anthem Blue Cross Life and Health Insurance Companys Essential Drug List.
Anthem blue cross blue shield prescription. Please request that your pharmacy contact Pharmacy Services at 8009221557 for assistance. You can also order and manage your prescriptions online by logging into your account. Anthem offers copays as low as 0 for our Prescription Drug Plans PDPs.
Your coverage has limitations and exclusions. HIP Plus and Hoosier Care Connect members can even have their medicines delivered to. Means Anthem Blue Cross and Blue Shield.
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. You can save money when your doctor prescribes medications on the drug list. Complete pharmacy information including access to formularies Preferred Drug Lists PDLs precertification information and other related resources is available through our Pharmacy Information page.
Log in to Availity. Fill your prescription drugs You can bring your Anthem Blue Cross Cal MediConnect Plan card and your prescription to a network pharmacy or a mail-order pharmacy. Our prescription drug benefits can offer potential savings when your physician prescribes medications on the drug list.
Before making a final decision please read the Plans Federal brochures Standard Option and Basic Option. This is a summary of the features of the Blue Cross and Blue Shield Service Benefit Plan. Our prescription drug benefits can offer potential savings when your physician prescribes medi cations on the drug list.
There are no copays for covered prescriptions. And with over 68000 national pharmacies youll find one close to you. Anthem Blue Cross and Blue Shield Healthcare Solutions is the trade name of Community Care Health Plan of Nevada Inc an independent.
For an updated formulary please. For new prescriptions have your doctor contact CVS Caremark toll-free at 1-800-378-5697 or have your doctor fax your prescription to CVS Caremark at 1-800-378-0323. Or contact the Customer Service number on your member ID card if you need assistance.
This document includes a list of the drugs formulary for our plan which is current as of 512021. Prescription Program Drug List To be used by members who have a three 3 tiered drug plan. The Anthem Blue Cross and Blue Shield Healthcare Solutions Anthem PDL includes all medicines covered by Medicaid.
Anthem Blue Cross Blue Shield prescription drug benefits include medications available on the Anthem Drug List. Health Insurance Medicare More Anthem Has You Covered Members will receive the COVID-19 vaccination at no cost. All benefits are subject to the definitions limitations and exclusions set forth in the Federal brochures.
You get a wide range of prescription drugs and over-the-counter medicines. Find the Anthem MediBlue Rx plan that fits your prescription. If your market doesnt use Availity for secure provider tasks please return to the Provider Overview page for additional state-specific.
Rocky Mountain Hospital and Medical Service Inc. Anthem works with IngenioRx to provide your pharmacy benefits. For example drugs used for cosmetic purposes usually are not covered.
For refills call toll-free at 1-877-FEP-FILL 1-877-337-3455. When it refers to plan or our plan it means Anthem MediBlue Rx Plus PDP. If your pharmacy is willing to accept assignment do not complete this form.
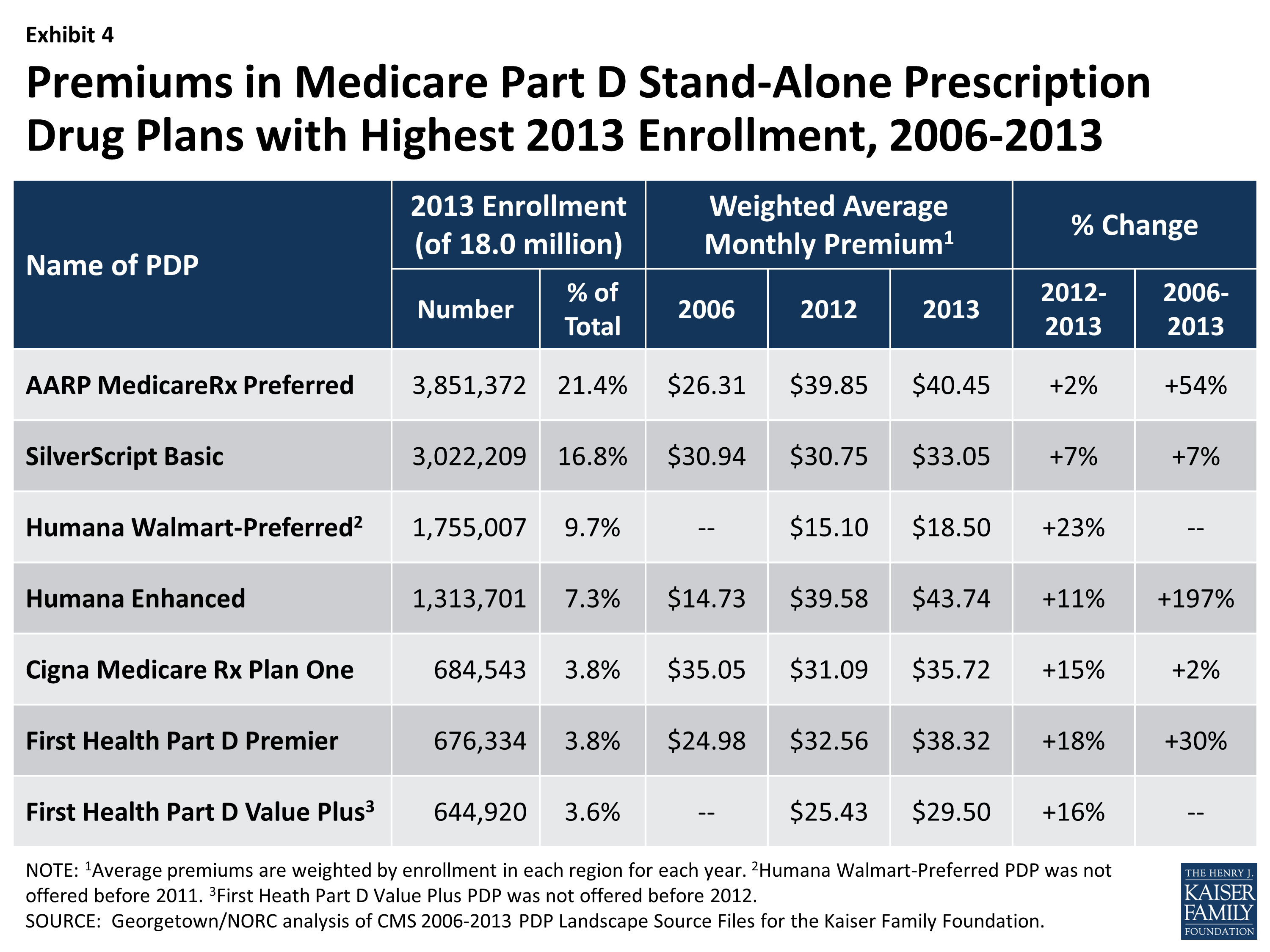
All of Anthems MediBlue Rx Part D plans have just 1 to 3 copays for generic tiers at preferred pharmacies after your deductible if it applies. The Availity Portal offers health care professionals free access to real-time information and instant responses in a consistent format regardless of the payer. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost.
Anthem Blue Cross Blue Shield. This is known as prior authorization PA. Anthem Blue Cross and Blue Shield Anthem prescription drug benefits include medications on the Anthem Preferred Drug List.
Anthem Blue Cross and Blue Shield Healthcare Solutions is the trade name of Community Care Health Plan of Nevada Inc an independent licensee of the Blue. As a Medicare member you may qualify for Extra Help with your Medicare prescription drug costs. Prescription Drug List by Tier.
Your request should include why a specific drug is needed and how much is needed. You may need to get approval from us for certain drugs. Assignment of these benefits to a pharmacy or any other party is void X.
Anthem Health Plans Inc. If youre new to Medicare Part D plans you can read more about prescription drug tiers and costs. Blue Cross and Blue Shield of Georgia Inc.
This list may be for you if you get your health insurance plan from an employer. Medicare Part D is Medicares Prescription Drug Coverage. Pharmacy Benefits Anthem BlueCross BlueShield Indiana Medicaid Pharmacy and prescription drugs Your benefits include a wide range of prescriptions and over-the-counter OTC medicines.
Signature of Member Date If allowed by law you may assign the payment of this claim to your pharmacy. HMO products underwritten by HMO Colorado Inc.