Your doctor will provide this form. Although some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form.
 Medicare Prior Authorization Forms Helpadvisor Com
Medicare Prior Authorization Forms Helpadvisor Com
You would think insurers would ease bureaucratic demands throughout a pandemic to ensure patients access to timely medically necessary care said AMA President Susan R.
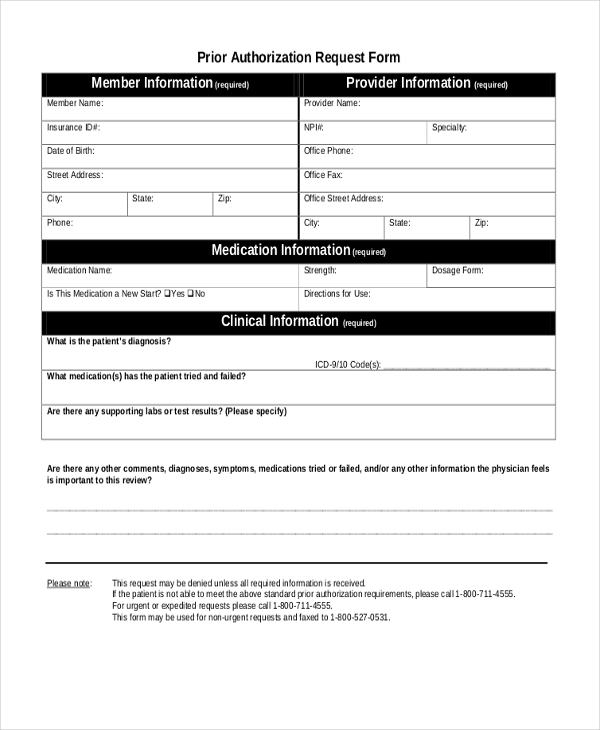
Do you need prior authorization for medicare. First you or your pharmacist should talk to your doctor. CMS believes prior authorization for certain hospital OPD services will ensure that Medicare beneficiaries continue to receive medically necessary care while protecting the Medicare Trust Fund from improper payments and at the same time keeping the medical necessity documentation requirements unchanged for providers. If prior authorization is needed for a certain service your provider must get it before giving you the service.
There may be another drug you can take that doesnt need prior authorization. For more information refer to Humana preauthorization automation on Availity. Look for a button labeled Click to Complete Questionnaire.
This means the automation feature is available for the service. Once the request gets approval coverage begins. Specifically the bill would establish an electronic prior authorization process require the implementation of a real-time decision system for items and services that are routinely approved mandate that MA plans provide more detailed reports on use of prior authorization to the US.
And create an authorization request as usual. Molina Healthcare does not require prior authorization for all services. You may not need a prior authorization.
Your doctor or other health care provider may recommend you get services more often than Medicare covers. For certain medical procedures services or medications your doctor or hospital needs advanced approval before your plan covers any of the costs. Check with your plan for more information.
During the COVID-19 pandemic Medicare Advantage Plans and Prescription Drug Plans may waive or relax prior authorization requirements. Through prior authorization and pre-claim review initiatives CMS helps ensure compliance with Medicare. It is needed before you can get certain services or drugs.
Prior authorization is when your provider gets approval from Molina Healthcare to provide you a service. If this happens you may have to pay some or all of the costs. If not you can start the approval process by calling the number on the back of your Blue Cross ID card.
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Answer the questions to receive an instant determination on your preauthorization. The Social Security Act didnt require any form of prior authorization for Medicare services in.
Prior Authorization is about cost-savings not care. In many cases pre-authorizations can be. Is there any gray area on whether Medicare or the insurance carrier would question the medical necessity.
You andor your prescriber must contact your plan before you can fill certain prescriptions. Private for-profit plans often require Prior Authorization. Visit the Preauthorization and notifications list online.
In this section you will find the tools and resources you need to help manage your practices prior authorization and notification requirements with program specific information available for Cardiology Oncology Radiology Clinical Pharmacy and Specialty Drugs. If you are currently using one of the drugs requiring prior authorization for medical necessity ask your doctor to choose one of the generic. You likely need prior authorization.
Sadly you would be wrong Learn how as COVID-19 peaked prior authorizations harmful burdens continued. Prior authorization for prescription drugs is required when your insurance company asks your physician to get specific medications approved by the insurance company. Does this service require preauthorization.
Your primary UnitedHealthcare prior authorization resource the Prior Authorization and Notification tool. As part of Medicare youll rarely need to obtain prior authorization. Original Medicare Medicare Supplement and prior authorization.
Centers for Medicare Medicaid Services including their. Authorization determinations are conducted for benefit determination or the application of medical necessity criteria or both. Prior Authorization and Pre-Claim Review Initiatives.
If you continue using one of these drugs without prior approval for medical necessity you may be required to pay the full cost. Below is a list of medicines by drug class that will not be covered without a prior authorization for medical necessity. For pre-Medicare health insurance policy owners pre-authorizations by an insurance carrier prior to many healthcare services is standard practice.
Prior authorization must be provided before the insurance company will provide full or any coverage for those medications. Why Do Insurance Companies Require Prior Authorization. Ask questions so you understand why your doctor is recommending certain services and whether Medicare will pay for.
Or they may recommend services that Medicare doesnt cover. Under Prior Authorization benefits are only paid if the medical care has been pre-approved by Medicare. The Centers for Medicare Medicaid Services CMS runs a variety of programs that support efforts to safeguard beneficiaries access to medically necessary items and services while reducing improper Medicare billing and payments.
You can also start the approval process by filling out and sending in a coverage determination form.
