There will be a payment reduction of 10 for not having an authorization. TRICARE Service Center number is 877-988-WEST or wwwtricaremil and explore option I want to You can enroll in or purchase a plan file or check or claim view referral and prior authorizations find a doctor change your primary care manger see whats covered compare plans or manage prescriptions.
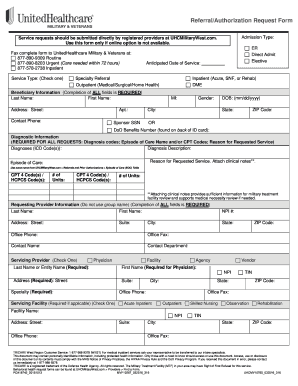 United Healthcare Referral Form Fill Out And Sign Printable Pdf Template Signnow
United Healthcare Referral Form Fill Out And Sign Printable Pdf Template Signnow
Check to see if we offer a Letter of Attestation you can attach instead of clinical documentation.
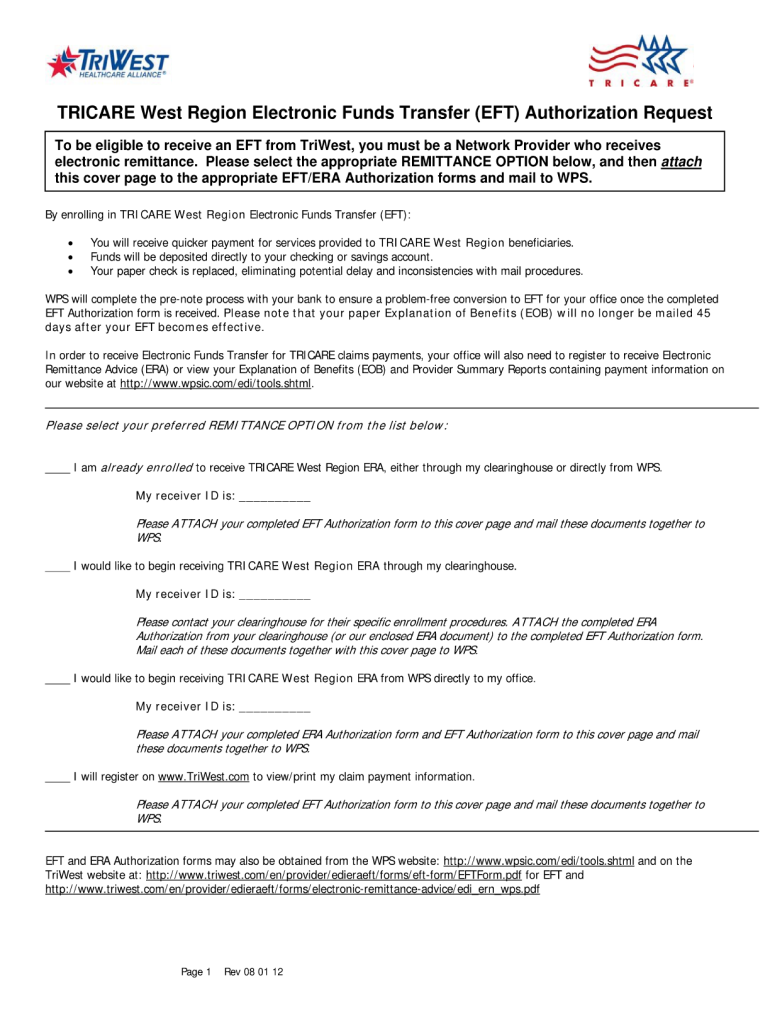
Tricare west prior authorization phone number. Search the TRICARE Formulary. Community Care Network Regions 4 and 5 Contact Center. Login for Secure Services Find the right place to log in for secure services like enrolling making appointments or checking referrals.
TriWest is pleased to offer options to help Veterans with hearing or speech disabilities communicate telephonically. When completing the referral always include the sponsors TRICARE ID diagnosis and clinical data explaining the reason for the referral. Our electronic prior authorization ePA solution is HIPAA-compliant and available for all plans and all medications at no cost to providers and their staff.
If you get a pre-authorization from the Nurse Advice Line for urgent care. Online authorization and referral tools offer quick and easy submission and status tracking of prior authorizations referrals and inpatient and discharge notifications. Claims Contact Information For detailed reimbursement or claims questions please call.
Prior authorizations for certain services andor procedures require Health Net Federal Services LLC HNFS review and approval prior to being provided. Tricares Preferred Method for Prior Authorization Requests. You must have prior authorization for all specialty care.
Check the TRICARE Formulary to see if you need prior authorization. Find the right phone number for what you need. Find a Phone Number Your Contacts East Region - Humana Military 1-800-444-5445.
Tips for creating referrals and authorizations. 877-CCN-TRIW 226-8749 Monday Friday. Choose the Provider menu and then choose Claims to speak to a TriWest claims representative.
It is our privilege to work alongside VA as we provide Veterans with access to high-quality health care through our. In your local time zone. Search the FAQs Find instant answers to the most frequently asked questions.
CoverMyMeds is the fastest and easiest way to review complete and track PA requests. Last Updated 452021 Find a TRICARE Plan Find a Doctor Find a Phone Number Your Contacts Express Scripts Inc. If the service has been performed greater than 5 business days ago the provider will need to submit a claim with supporting documentation for a review to the claims department via the website or via fax at 608-301-2114 or 608-301-3100.
If you are unsure if you need urgent care you can call the Nurse Advice Line at 1-800-TRICARE 800-874-2273 option 1. West Region - Health Net Federal Services. Find a Claims Address Find the right address for medical pharmacy or dental claims.
The Prior Authorization Referral and Benefit Tool will prompt you to answer a few simple questions about the beneficiary the provider performing the service and the service itself in order to determine if an approval from Health Net Federal Services LLC HNFS is required prior to a beneficiary seeking care. Express Scripts will contact you. HNFS posts these documents electronically to the Secure Inbox where they can viewed online andor printed.
All Other Beneficiaries Enrolled in a TRICARE Prime Plan. TriWest Healthcare Alliance is On a Mission to Serve our nations Veterans and military community in partnership with the Department of Veterans Affairs VA in administering the Veterans Choice Program VCP and Veterans Affairs Patient-Centered Community Care PC3 program. What does it mean to get prior authorization.
View a tutorial for a step-by-step process of entering a new request andor checkupdate an existing referral or authorization.