This is extremely important to know especially for people being treated for cancer. There are hundreds of different medications with more becoming available every day.
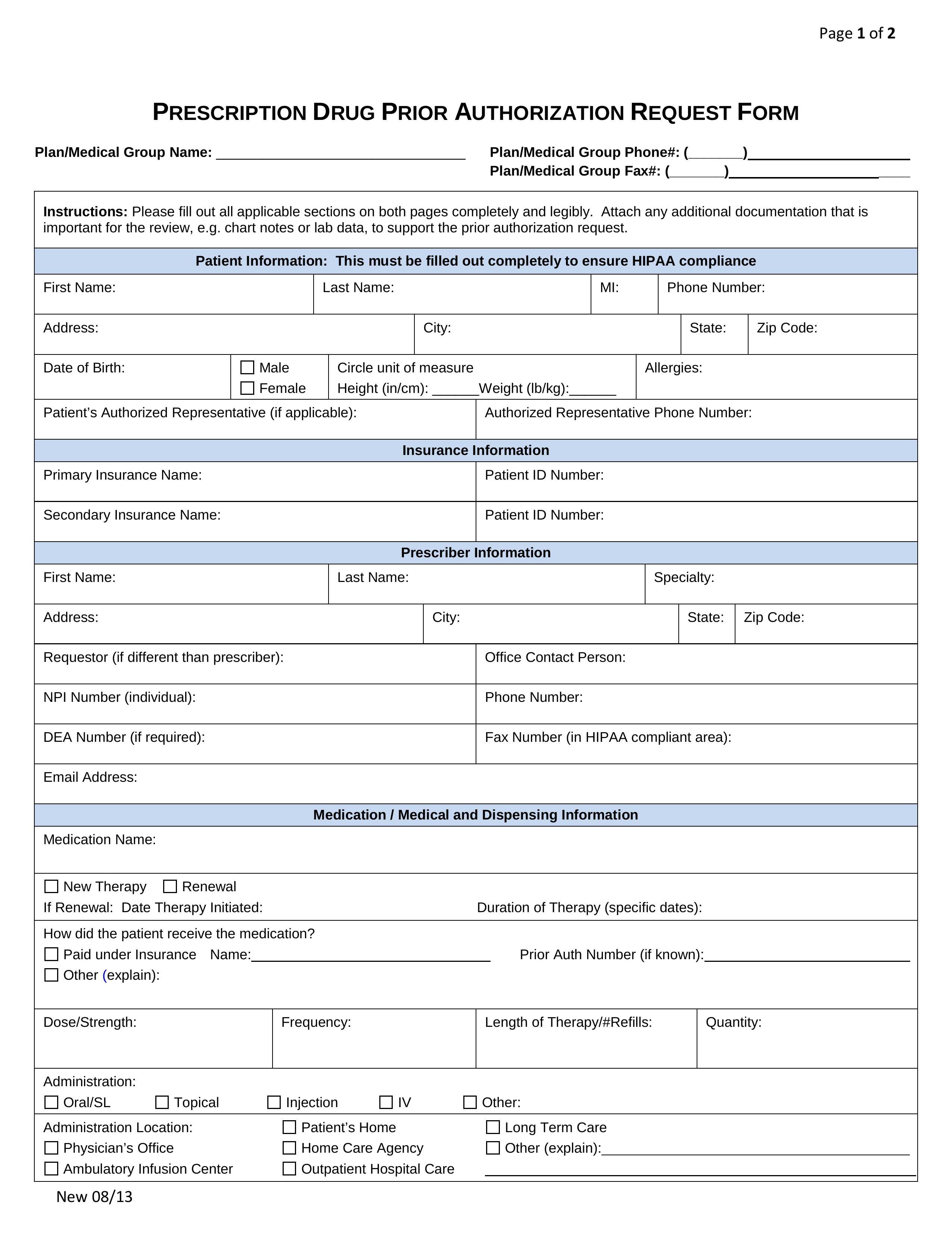 Free Prior Rx Authorization Forms Pdf Eforms
Free Prior Rx Authorization Forms Pdf Eforms
Submitting a request for prior authorization A request must be submitted and approved in advance for medications requiring a prior authorization before the drugs may be covered by Humana.

Pre authorization for medication. If a PA is needed locate the process for submitting and obtain any required prior authorization forms. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Without this prior approval your health insurance provider may not pay for your medication or operation leaving you with the bill instead.
Health insurance companies use prior authorization to verify that a certain drug procedure or treatment is medically necessary before it is done or prescribed. Its also a way for your health insurance company to manage costs for otherwise expensive medications. Prior authorization is a requirement that your physician obtains approval from your healthcare provider before prescribing a specific medication for you or to performing a particular operation.
You may find these on. Blue Cross Blue Shield of Michigan and Blue Care Network use prior authorization to make sure you get the right medication. Certain specialized services and prescription drugs require a prior authorization or inpatient notification before being rendered to patients and members.
Prior authorization PA is often used with expensive prescription drugs. Prior authorization PA is a requirement that your physician obtain approval from your health insurance plan to prescribe a specific medication for you. PA Forms for Physicians When a PA is needed for a prescription the member will be asked to have the physician or authorized agent of the physician contact our Prior Authorization Department to answer criteria questions to determine coverage.
Prior authorization is designed to help prevent you from being prescribed medications you may not need those that could interact dangerously with others you may be taking or those that are potentially addictive. PA is a technique for minimizing costs. If you cant submit a request via telephone please use our general request form or one of the state specific forms below and fax it.
As part of this effort we retired certain fax numbers for medical prior authorization requests in 2019 and asked you to use the Prior Authorization and Notification tool on Link the same website you use to check eligibility and benefits manage claims and update your demographic information. Health insurance companies use the prior authorization or pre-approval process to verify that a certain drug procedure or service is medically necessary BEFORE it is done or the prescription is filled. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Depending on a patients plan you may be required to request a prior authorization or precertification for any number of prescriptions or services. Prior Authorization can ensure proper patient selection dosage drug administration and duration of selected drugs. Check your plans policy documents and formulary to see if any of your treatments require a PA.
How Do I Get Prior Authorization for a Medication. Prescribers can submit their requests to Humana Clinical Pharmacy Review HCPR in the following ways. A full list of CPT codes are available on the CignaforHCP portal.
How to request precertifications and prior authorizations for patients. This information explains what it means if your doctor has prescribed a medication that needs prior authorization. Pharmacy Prior Authorization Forms Preferred Drug List Health Resources.
Prior Authorization Resources Please call us at 8007532851 to submit a verbal prior authorization request if you are unable to use Electronic Prior Authorization.