Especially BPH since Flomax and Proscar are generally approved as they were by my company before my Urologist switched me to Cialis 5mg. Blue Care Network reviews all physician and member requests to determine if the drug is medically necessary and if there are equally effective alternative drugs on the formulary.
 See 2020 Prescription Drug Changes Blue Cross And Blue Shield Of Illinois
See 2020 Prescription Drug Changes Blue Cross And Blue Shield Of Illinois
Generic equivalent drugs mandatory when available.
Does bcbs cover ed drugs. Drugs that need prior authorization and step therapy. We will notify both you and your doctor in writing if the request is denied. Blue Cross Blue Shield BCBS health insurance does cover rehab for drug and alcohol addiction.
Learn more about prior authorizations here. The PDL is a list showing the drugs that can be covered by the plan. The fact that Cialis is FDA approved as a treatment for both ED and BPH is a strong reason for insurance to approve it.
If you have a health condition that may jeopardize your life health or keep you from regaining function or your current drug therapy uses a non-covered drug you your prescriber or your authorized representative may be able to ask for an expedited review process. Preventive drugs per the Affordable Care Act. A drug thats not in our formulary sometimes called a drug list may require prior authorization.
But youll get more information about them in the specialized lists. If you have a health condition that may jeopardize your life health or keep you from regaining function or your current drug therapy uses a non-covered drug you or your prescriber may be able to ask for an expedited review process. Certain drugs may require prior authorization for the plan to pay.
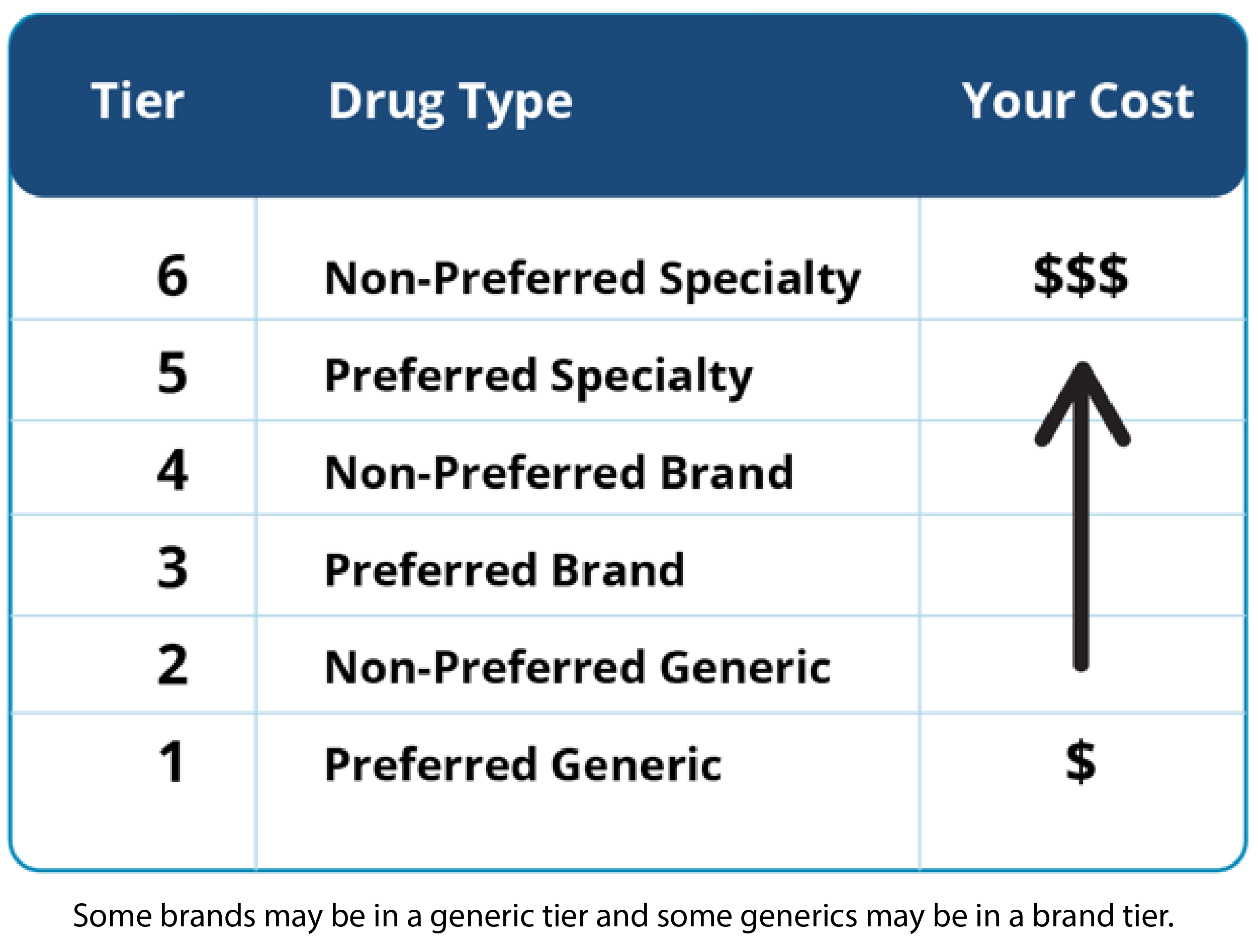
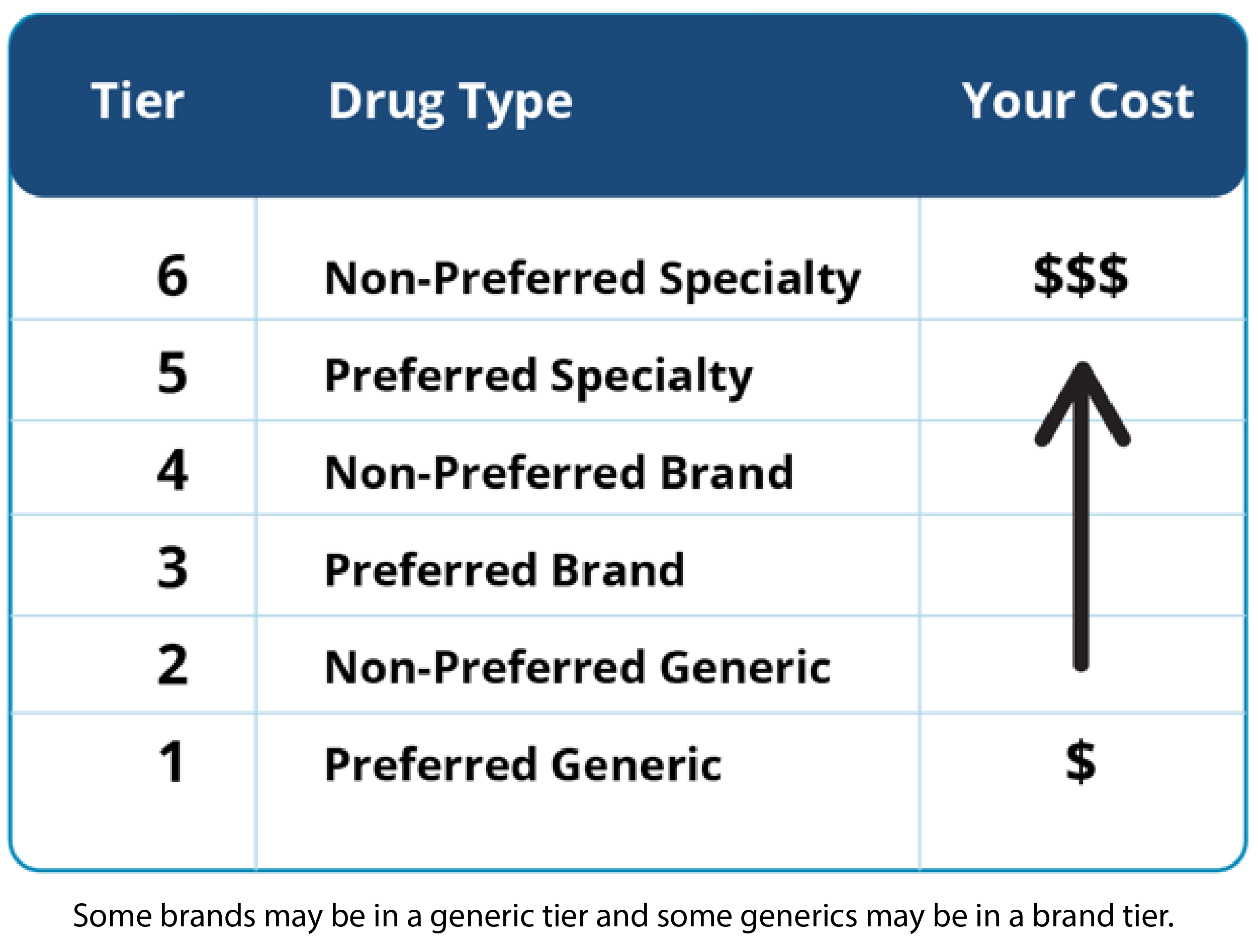
Tier 4 and 5 specialty drugs are limited to a. You can request continued coverage of a non-covered drug through our clinical exception program for members when there is a medical basis for the member not being able to take any of the covered drugs from the same therapeutic class. Most plans also have specialized drug lists just for.
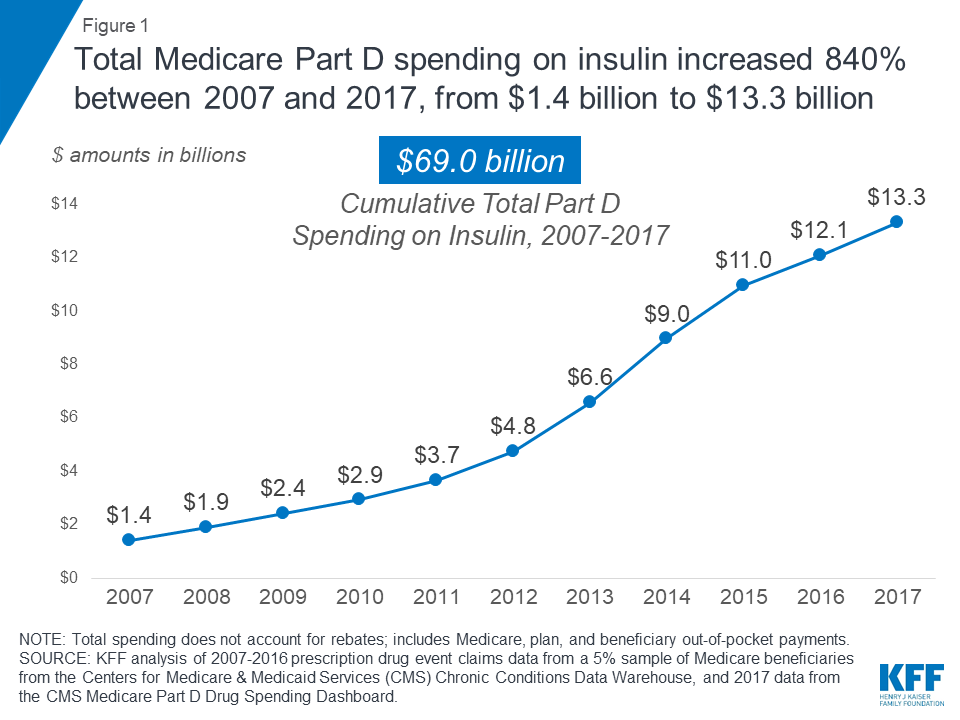
Open Enrollment runs from October 15 through December 7 and it provides an annual opportunity for Medicare-eligible consumers to review and make changes to their Medicare coverage. You can go to Medicaregovs Find a Medicare Plan tool to compare rates and drug. ED medications are not generally covered by Medicare Part D plans but Revatio for PAH is covered by most plans.
Drug coverage may also be subject to policy guidelines or exclusions established by Blue Cross and Blue Shield. This means before your plan will cover a particular drug you must show that you meet specific criteria for that drug. BCBSIL will let you your prescriber or authorized representative know the coverage decision within.
Drug Class Excluded Medications Preferred Alternatives MUSCULOSKELETAL RHEUMATOLOGY Gout Therapy COLCHICINE CAPSULES colchicine tablets MITIGARE Nonsteroidal Anti-Inflammatory Drugs NSAIDs DICLOFENAC 35 MG CAPSULES INDOMETHACIN 20 MG CAPSULES KETOROLAC NASAL SPRAY TIVORBEX ZIPSOR. The following guidelines are meant to help members understand the requirements related to their drug coverage. 60 of our allowance 75 minimum for up to a 30-day supply.
Also some drugs may only be covered for members within. It obviously depends on your insurance. This plan uses a Preferred Drug List PDL.
If your prescription drug isnt covered. Any legal requirements or group specific benefits for coverage will supersede this eg. BCBSTX will let you and your prescriber know the coverage decision within 24 hours after they receive your request for an.
Some plans may exclude coverage for certain agents or drug categories like those used for erectile dysfunction or weight loss. 210 minimum for a 31 to 90-day supply. Open enrollment is coming up again in Nov and would like to try and find a company that covers it.
Drugs that have a 15-day quantity limit. The 20 mg vs 5 mg daily regimen. Tier 4 Preferred specialty.
Physicians or their representatives may call BCBSMA Pharmacy Operations department to request a review for formulary exception for. Mine covers Cialis 5mg daily. Weight Height BMI Weight.
However if you elect to receive Part D coverage after your Initial Enrollment Period. As a Blue Cross Community Health Plans SM member you have coverage for selected generic prescriptions brand name prescriptions over-the-counter OTC drugs and selected medical supplies. I have Highmark BCBS and they will NOT cover it nor does UPMC.
Non formulary medications are covered when a formulary exception request is submitted to BCBSMA Pharmacy Operations and step criteria below are met Coverage Criteria for initiation and continuation of therapy shall include. I got the 30 day trail from my doctor and loved it but had to stop because i cant afford 900 every month. Find your drug lists.
-preferred brand drugs Tier 3 60 copayprescription days 1-30 120 copaydays 31-60 180 copaydays 61-90 Specialty drugs Tier 4 20 coinsurance 100 copay minimum 150 copay maximum Covers up to a 30 -day. Tier 5 Non-preferred specialty. RC Claim Assist provides an inclusive overview of medical drug products and a calculation tool to identify the correct National Drug Code and CPT codes to bill along with the.
BCBS is a large and well known insurance provider that is accepted at many addiction treatment facilities including American Addiction Centers. Prior authorizations are handled by your healthcare professionals office. Tier 3 Non-preferred brand.
If your medication is in this category getting a prior authorization will result in coverage. This includes the opportunity to select or make changes to Prescription Drug Coverage Part D. Or it might not be a covered benefit under your drug plan.
These drugs are included on your plans main drug list. Maintenance medications are those drugs you may take on an ongoing basis for conditions such as high blood pressure diabetes or high cholesterol. RC Claim Assist is a web-based resource available to Blue Cross Blue Shield of Michigan and Blue Care Network contracted providers who bill for drugs covered under the medical benefit.