Several of these sites are now also accepting walk-ins. City of San Diego Vaccination Program.
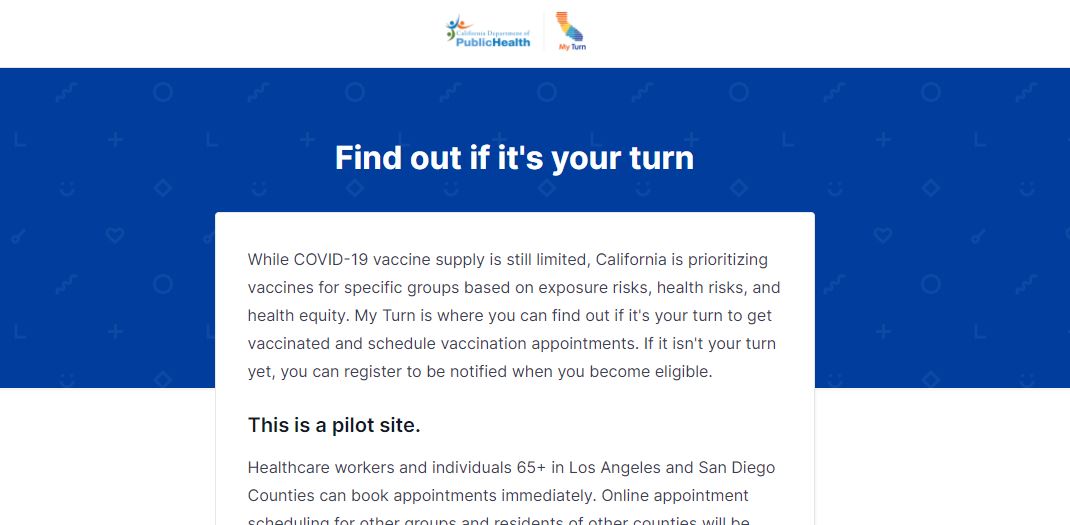 Ca Launches Myturn Vaccine Appointment Site After Frustrations Abound In Riverside County Other Locations Kesq
Ca Launches Myturn Vaccine Appointment Site After Frustrations Abound In Riverside County Other Locations Kesq
5130 Canyon Crest Drive 92182.

Myturn vaccine san diego. SAN DIEGO KGTV Demand for the COVID-19 vaccine is going up now that all adults are eligible in California. If you have a Facebook account you may want to join the San Diego Vaccine Hunters group where more than 6000 people ask and answer questions about how to book an appointment. The walk-thru vaccination site is located in lot 13.
As of Tuesday 1047512 San Diego County residents have had at least one shot. You will schedule your second dose on site during your first dose. Start by visiting myturncagov.
Viejas Arena Lot 13. The pool of eligibility is set to expand on April 15 when all San Diegans 15 and over will be eligible for the shot. Three County locations are now open 100 PM - 800 PM no appointment needed.
Everyone 16 years and older who lives works or goes to school in San Diego County can get a vaccine at no cost. San Diego College Area Vaccine Site at San Diego State University SDSU. ABC 10News looks at what you can do to secure an appointment.
That includes the regions newest vaccine location run by the county in partnership with San Diego State University at the Viejas Arena. MyTurn COVID-19 Vaccine Website Launches In San Diego County - San Diego CA - The MyTurn system is operating on a trial basis for residents in Los Angeles and San Diego counties. Heres how to register.
If you want to make an appointment at one of the smaller county-run sites you can do so through an online system called MyTurn myturncagov. You do not need an appointment but they are available if preferred. Click here to see campus map.
Sami Gallegos press secretary for Californias COVID-19 Vaccine Task Force told CalMatters that pediatricians and other doctors who treat children will not be forced to use MyTurn. MyTurn was designed for real Californians to make vaccine appointments and intentionally makes it hard for computers to automate the booking process said Darrel Ng senior communications advisor. My Turn a state contractor web-based scheduler being used to book vaccine appointments is currently being used in LA and San Diego as a pilot program for the state.
For any issues contact SDFCovid19sandiegogov. For more details click here. You will then receive a reminder email within 7-10 days following your initial vaccination.
SAN DIEGO The county says vaccines are available without an appointment at three sites in San Diego County Wednesday because of an issue with the MyTurn site. Santa Clara County kept its own vaccine appointment system making its clinics and the Levi Stadium mass vaccination site far less visible on MyTurn. You do not need health insurance to be vaccinated.
Select your language and click the blue button to check your eligibility. Designated parking in parking structure 12 PS12 level 2 only. One of the main.
The new scheduling and data system called My Turn launched in Los Angeles and San Diego counties with state leaders hoping for a statewide. San Diego County officials recently signed a memorandum of understanding with the state that will allow the region to continue its coronavirus vaccine rollout as part of a network of providers.