Procedures must be consistent with established medical practice in treatment of infertility. Gateway Health provides coverage under the medical-surgical benefits of the Companys Medicaid.
Https Ga Beerepurves Com Brokerworkspace Tools Benefits Infertilitybenefits Sg Pdf
Additionally does Medicaid cover a Panniculectomy.
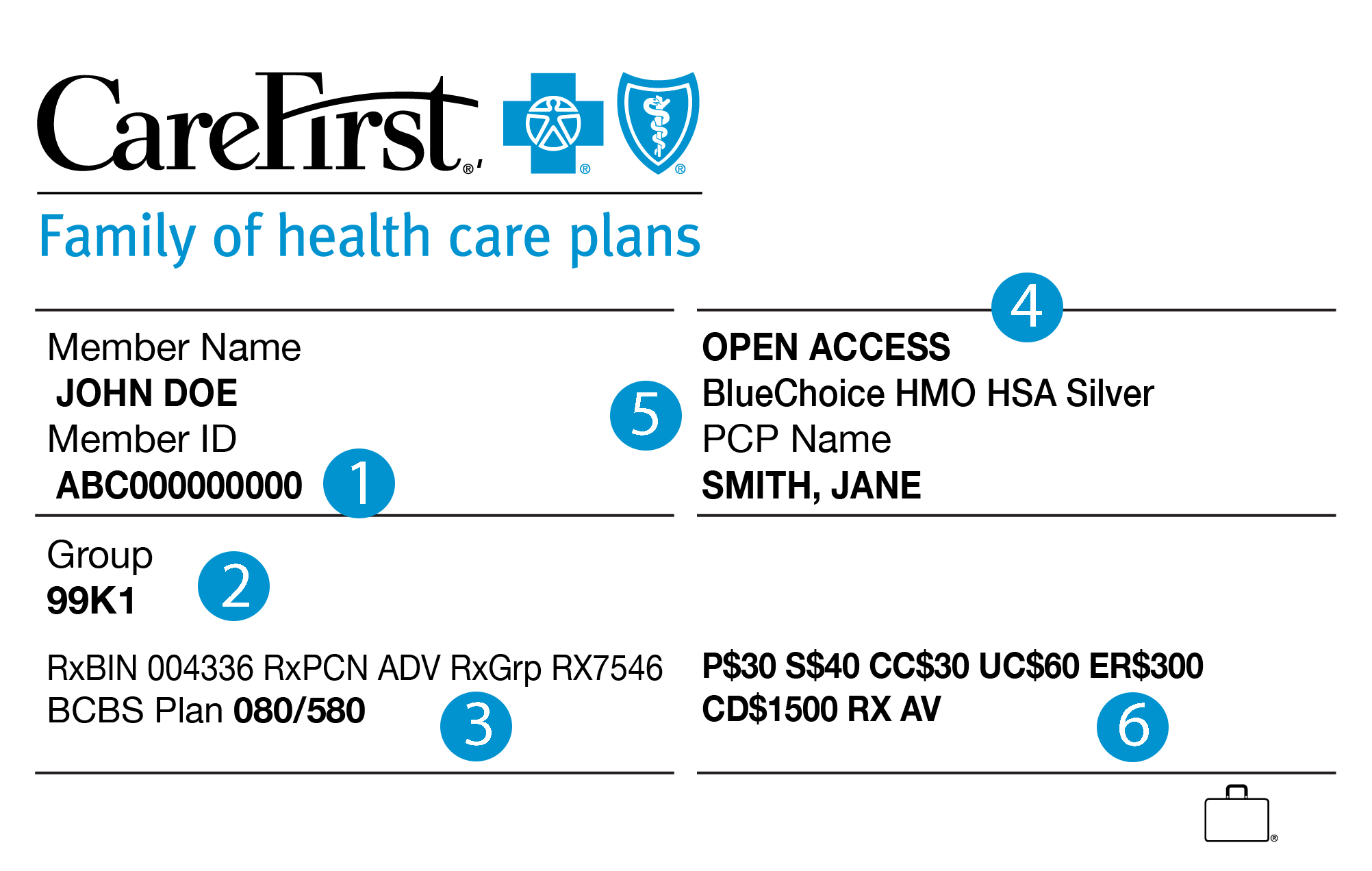
Does blue cross blue shield insurance cover ivf. Another important requirement that Blue CrossBlue Shield sets out is that the sperm utilized for any IUI or IVF procedures must be that of the patients spouse. Please check the member benefit language regarding the benefits. The Blue Cross Blue Shield Association is a national association of 36 independent community-based and locally operated Blue Cross Blue Shield companies.
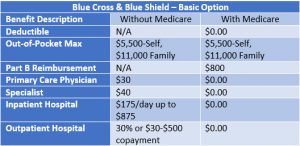
Blue Cross Blue Shield insurance does cover testing. Covered Infertility Benefits up to the lifetime maximum None Infertility Benefits Blue Shield Payment Covered Infertility Benefits up to the lifetime benefit maximums as described in this Supplement 50 of the Allowable Amount 1 Infertility Benefits are only covered when provided by Preferred or Participating Providers. Are frequently excluded from coverage.
Blue Cross Blue Shield policies are offered through the Florida state insurance exchange created by the Affordable Care ActAccording to the Affordable Care Act all Marketplace plans are required to provide coverage for essential health benefits including. Empire Blue Cross Blue Shield infertility coverage. Also know will Blue Cross Blue Shield pay for Panniculectomy.
So I paid roughly 3k for the meds out of pocket for 1 cycle. We ha be Blue Cross Blue Shield and it has a lifetime infertility coverage of 10000 but IVF is not covered at all. I have it in Fl and i have a max coverage lifetime for fertility of 10000 and covers IUI IVF or ZIFT at 50.
For IVF services BCBSA gives coverage to members if only specified in the member contract. The scope of this analysis included. It did help with IUIs though and we had awesome drug coverage that saved us quite a bit.
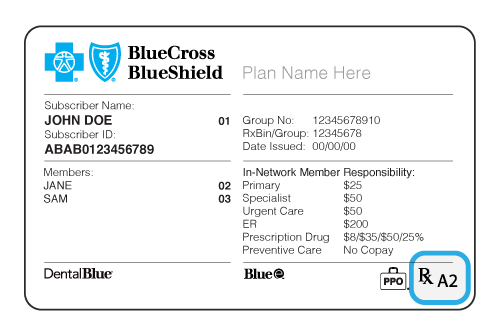
This law requires insurance policies that cover more than 25 people to cover costs of the diagnosis and treatment of infertility. Thankyou so much ZenGirl. These services are only covered if the members benefit booklet identifies Artificial insemination AI Intrauterine Insemination IUI andor In Vitro fertilization IVF as covered services.
6 Blue Distinction Centers for Fertility Care Program Selection Criteria Cost Data Sources and Defining the Episodes Cost of Care evaluation was based on a nationally consistent analysis of Blue Plan healthcare claims data. Presumptive and definitive qualitative or quantitative drug testing methods after a drug has been detected through a screening or presumptive test if a provider has submitted a written. Yes in Illinois benefits will be provided the same as your benefits for any other condition for Covered Services rendered in connection with the diagnosis andor treatment of infertility including but not limited to in-vitro fertilization uterine embryo lavage embryo transfer artificial insemination gamete intrafallopian tube transfer zygote intrafallopian tube transfer low tubal ovum transfer and.
Other Blue Cross Blue Shield Plans. BCBSNC will provide coverage for Panniculectomy when it is determined to be medically necessary because the medical criteria and guidelines shown below are met. Normally it would have been a.
These services are covered only when authorized by Blue Shield and provided by a Participating Provider Shield Spectrum PPO Savings Plus Plans and Active Choice Plans. The only exclusion was donor sperm. The company covers all aspects of healthcare including infertility treatments such as IVF and IUI for its policyholders.
Blue Cross Blue Shield BCBS will sometimes issue plans that cover infertility treatment including IVF when required by state law or when requested by an employer group. As with most medical insurance fertility treatments are not covered. Also our wash for our IUI was covered too.
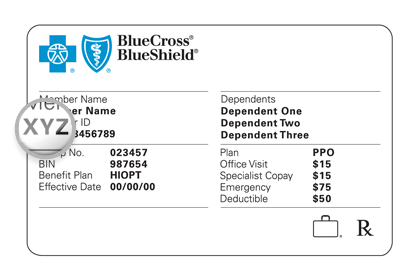
It it is best to work with your HR department andor call Empire Blue and get a run down of which infertility options your company has contracted from them. Our most expensive IVF medication cycle was 285. Items that are covered include the following.
Labs and ultrasounds are covered. BUTThey will pay 1000 per year for lab tests and x-rays which includes ultrasounds for diagnostic purposes not while pregnant sperm function analysis not the basic semen analysis but the super duper one the fertility clinics do. There is no fertility coverage for those outside of this type of relationship.
Sep 17 2015 at 906 AM MsSamantha1106 Blue Cross and Blue Shield of FL covered all diagnostics and had a 10k lifetime maximum for IVF but covered no meds. Because of this different companies have different policies for lipedema surgery coverage. My plan - Arkansas Blue Cross Blue Shield covered up to 10000 on fertility treatments up to and including IVF.
Drug testing coverage is limited to 20 tests per the calendar year unless the insured seeks special approval. These services are only covered when the group adds Additional Infertility Treatment Benefits tothe health plan. The coverage really depends on which options your company buys from Empire Blue.
However Blue Cross Blue Shield is a national federation of affiliated companies using this trade name. I also have BC--PPO NYwith 13000 coverage. I had to pay 10 of allowable charges after my deductible was met.
Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies. The Blue Cross Blue Shield Association BCBSA stands out as one of the most recognized insurance providers in the US. As of November 24 2020 Health Care Service Corporation the second-largest Blue Cross Blue.
The law defines infertility as the inability to get pregnant after.