Like an HMO your care is covered only if you see a provider in the plans network unless its an emergency as defined by the plan. One of the most significant advantages to an EPO is participants dont need a referral from a primary care physician to see a specialist.
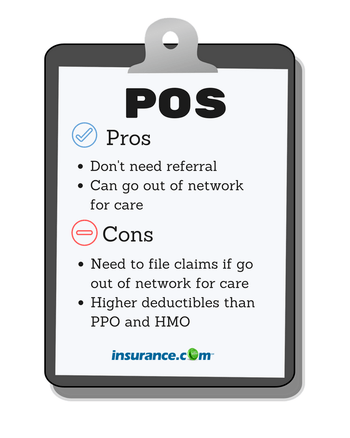 Hmo Vs Ppo Vs Other Plans What S The Difference Insurance Com
Hmo Vs Ppo Vs Other Plans What S The Difference Insurance Com
An exclusive provider organization or EPO is a health insurance plan that only allows you to get health care services from doctors hospitals and other care providers who are within your network.
What does epo mean in health insurance. EPO health insurance got this name because you have to get your health care exclusively from healthcare providers the EPO contracts with or the EPO wont pay for the care. A type of managed care health insurance EPO stands for exclusive provider organization. Members however may not need a referral to see a specialist.
Organization EPO Exclusive Provider Organization and HDHP High Deductible Health Plan. Like HMOs EPOs cover only in-network care but networks are generally larger than for HMOs. They may or may not require referrals from a primary care physician.
The only exception is that emergency care is usually covered. EPO stands for Exclusive Provider Organization plan. EPO is just one of several common health insurance plans offered by employers.
However there are some exceptions to this rule such as if the patient experiences a medical emergency. A provider network can be made up of doctors hospitals and other health care providers and facilities that have agreed to offer negotiated rates for services to insureds of certain medical insurance plans. The plan offers a local network of doctors and specialists in your area in.
Many health insurance cards show the amount you will pay. There are a number of different types of networks with HMO PPO EPO and POS being some of the most common. You must stick to providers on that list or the EPO wont pay.
EPOs generally offer a little more flexibility than an HMO and are generally a bit less pricey than a PPO. An EPO is a managed care plan in which services are only covered if the patient sees a doctor specialist or hospital within the plans network. An Exclusive Provider Organization or EPO is a type of health insurance plan in which members must utilize doctors and providers within the EPO network except in case of a medical emergency.
As a member of an EPO you can use the doctors and hospitals within the EPO network but cannot go outside the network for care. They generally dont cover care outside the plans provider network. EPO health insurance stands for Exclusive Provider Organization.
Exclusive Provider Organization EPO health plans are similar to Health Maintenance Organizations HMOs as they do not cover care outside of the plans provider network. An Exclusive Provider Organization plan EPO is similar to an HMO plan in that it has a limited doctor network and no out-of-network coverage but it is similar to a PPO plan in that you dont have to designate a primary care physician upon applying and you dont need a referral to see a specialist. Under an EPO plan you can go to a doctor andor hospital that is in-network.
If you choose an. Exclusive provider organizations EPOs are a lot like HMOs. There are no out-of-network benefits.
Your insurance will not cover any costs you get from going to someone outside of that network. Exclusive Provider Organization EPO combines elements of PPOs and HMOs. An EPO plan may be right for you if.
This allows people who have trouble getting insurance that allows them to afford care to have a regular physician who knows their case and can advise them on what they should do regarding their ongoing health care. An EPO Exclusive Provider Organization plan lets you use any of the providers within the EPO network. Exclusive Provider Organization EPO EPOs got that name because they have a network of providers they use exclusively.
If its not an emergency and you see an out-of-network provider you will have to pay the full cost out of your pocket. However there are no out-of-network benefits - meaning you are responsible for 100 of expenses for any visits to an out-of-network doctor or hospital. An Exclusive Provider Organization EPO is a lesser-known plan type.
An EPO or exclusive provider organization is a bit like a hybrid of an HMO and a PPO. However if you choose out-of-network health care providers it usually will not be covered. An Exclusive Provider Organization EPO is a health plan that offers a large national network of doctors and hospitals for you to choose from.
However an EPO generally wont make you get a referral from a primary care physician in order to visit a specialist. Like a PPO you do not need a referral to get care from a specialist.
 What Does Epo Mean In Health Insurance Business Benefits Group
What Does Epo Mean In Health Insurance Business Benefits Group
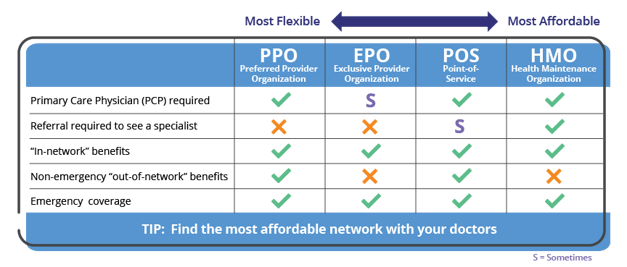
 What Type Of Health Plan Works Best For Me Choosing The Right Plan Independence Blue Cross
What Type Of Health Plan Works Best For Me Choosing The Right Plan Independence Blue Cross
 What Is An Epo Health Insurance Plan
What Is An Epo Health Insurance Plan
 Epo Vs Ppo Difference And Comparison Diffen
Epo Vs Ppo Difference And Comparison Diffen
 What S The Difference Between Hmo Ppo Pos And Epo Insurance Justworks
What S The Difference Between Hmo Ppo Pos And Epo Insurance Justworks
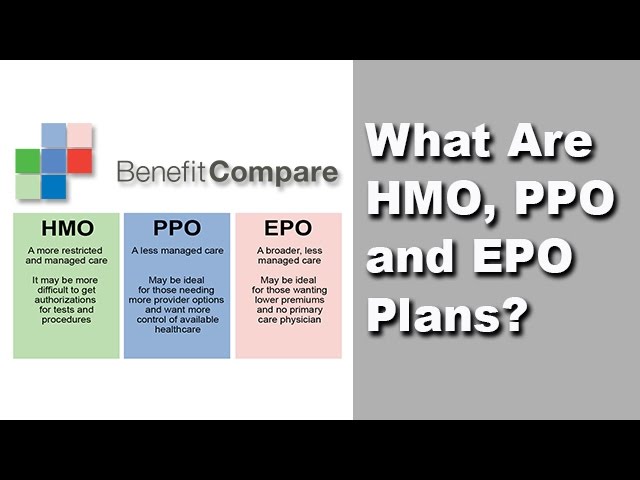 What Are The Differences Between Hmo Ppo And Epo Health Plans New Youtube
What Are The Differences Between Hmo Ppo And Epo Health Plans New Youtube
 Know Your Options Individual Health Insurance In Tennessee
Know Your Options Individual Health Insurance In Tennessee
 Hmo Vs Epo Vs Ppo Which Is Better What S The Cheapest
Hmo Vs Epo Vs Ppo Which Is Better What S The Cheapest
Epo Health Plans Independence Blue Cross Ibx
 What Does Epo Mean In Health Insurance Business Benefits Group
What Does Epo Mean In Health Insurance Business Benefits Group
 Understanding The Difference Between In Network And Out Of Network Provider Coverage
Understanding The Difference Between In Network And Out Of Network Provider Coverage
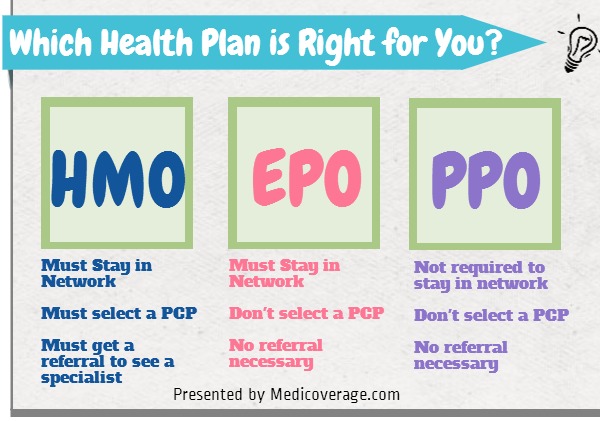 Hmo Vs Epo Vs Ppo Explained Medicoverage Com
Hmo Vs Epo Vs Ppo Explained Medicoverage Com
 What Does Epo Mean In Health Insurance Business Benefits Group
What Does Epo Mean In Health Insurance Business Benefits Group
 The Insurance Basics Cf Foundation
The Insurance Basics Cf Foundation
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.